Coronaviruses
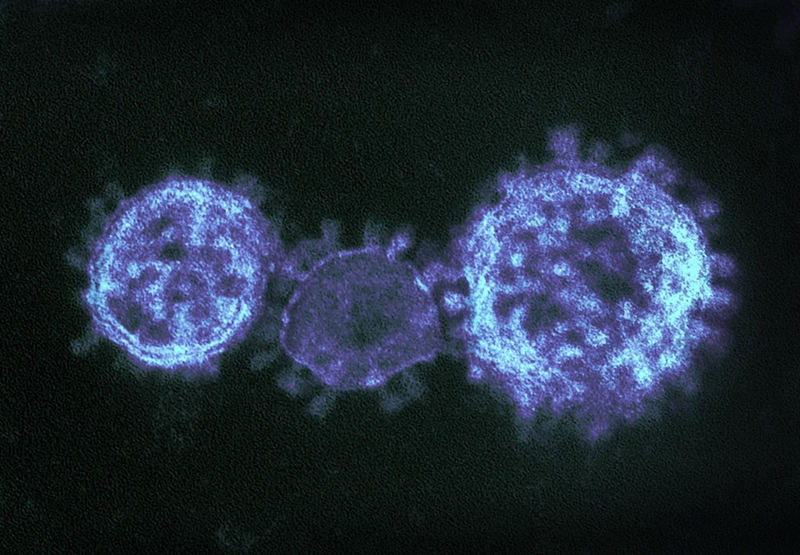
Coronaviruses are a large family of viruses that can infect a range of hosts. They are known to cause diseases including the common cold, Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) in humans.
In January 2020, China saw an outbreak of a new coronavirus strain now named SARS-CoV-2. Although the animal reservoir for the SARS and MERS viruses are known, this has yet to have been confirmed for SARS-CoV-2. All three strains are transmissible between humans.
To allow the widest possible distribution of relevant research, the Microbiology Society has brought together articles from across our portfolio and made this content freely available.
Image credit: "MERS-CoV" by NIAID is licensed under CC BY 2.0, this image has been modified.
Collection Contents
-
-
Validation of saliva sampling as an alternative to oro-nasopharyngeal swab for detection of SARS-CoV-2 using unextracted rRT-PCR with the Allplex 2019-nCoV assay
More LessIntroduction. The current severe acute respiratory syndrome-associated coronavirus-2 (SARS-CoV-2) pandemic has stressed the global supply chain for specialized equipment, including flocked swabs.
Hypothesis. Saliva could be a potential alternative specimen source for diagnosis of SARS-CoV-2 infection by reverse-transcriptase PCR (RT-PCR).
Aim. To compare the detection efficiency of SARS-CoV-2 RNA in saliva and oro-nasopharyngeal swab (ONPS) specimens.
Methodology. Patients recruited from hospital provided paired saliva and ONPS specimens. We performed manual or automated RT-PCR with prior proteinase K treatment without RNA extraction using the Seegene Allplex 2019 nCoV assay.
Results. Of the 773 specimen pairs, 165 (21.3 %) had at least one positive sample. Additionally, 138 specimens tested positive by both sampling methods. Fifteen and 12 cases were detected only by nasopharyngeal swab and saliva, respectively. The sensitivity of ONPS (153/165; 92.7 %; 95 % CI: 88.8–96.7) was similar to that of saliva (150/165; 90.9 %; 95 % CI: 86.5–95.3; P=0.5). In patients with symptoms for ≤ 10 days, the sensitivity of ONPS (118/126; 93.7 %; 95 % CI: 89.4–97.9) was similar to that of saliva (122/126; 96.8 %; 95 % CI: 93.8–99.9 %; P=0.9). However, the sensitivity of ONPS (20/22; 95.2 %; 95 % CI: 86.1–100) was higher than that of saliva (16/22; 71.4 %; 95 % CI: 52.1–90.8) in patients with symptoms for more than 10 days.
Conclusions. Saliva sampling is an acceptable alternative to ONPS for diagnosing SARS-CoV-2 infection in symptomatic individuals displaying symptoms for ≤ 10 days. These results reinforce the need to expand the use of saliva samples, which are self-collected and do not require swabs.
-
-
-
The value of repeat patient testing for SARS-CoV-2: real-world experience during the first wave
More LessIntroduction. Reports of false-negative quantitative reverse transcription PCR (RT-qPCR) results from patients with high clinical suspension for coronavirus disease 2019 (COVID-19), suggested that a negative result produced by a nucleic acid amplification assays (NAAs) did not always exclude the possibility of COVID-19 infection. Repeat testing has been used by clinicians as a strategy in an to attempt to improve laboratory diagnosis of COVID-19 and overcome false-negative results in particular.
Aim. To investigate whether repeat testing is helpful for overcoming false-negative results.
Methods. We retrospectively reviewed our experience with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing, focusing on the yield of repeat patient testing for improving SARS-CoV-2 detection by NAA.
Results. We found that the yield from using repeat testing to identify false-negative patients was low. When the first test produced a negative result, only 6 % of patients tested positive by the second test. The yield decreased to 1.7 and then 0 % after the third and fourth tests, respectively. When comparing the results produced by three assays, the Centers for Disease Control and Prevention (CDC) SARS CoV-2 RT-qPCR panel, Xpert Xpress CoV-2 and ID NOW COVID-19, the ID NOW assay was associated with the highest number of patients who tested negative initially but positive on repeat testing. The CDC SARS CoV-2 RT-qPCR panel produced the highest number of indeterminate results. Repeat testing resolved more than 90 % of indeterminate/invalid results.
Conclusions. The yield from using repeat testing to identify false-negative patients was low. Repeat testing was best used for resolving indeterminate/invalid results.
-
-
-
Vesicular stomatitis virus pseudotyped with severe acute respiratory syndrome coronavirus spike protein
More LessSevere acute respiratory syndrome coronavirus (SARS-CoV) contains a single spike (S) protein, which binds to its receptor, angiotensin-converting enzyme 2 (ACE2), induces membrane fusion and serves as a neutralizing antigen. A SARS-CoV-S protein-bearing vesicular stomatitis virus (VSV) pseudotype using the VSVΔG* system was generated. Partial deletion of the SARS-CoV-S protein cytoplasmic domain allowed efficient incorporation into VSV particles and led to the generation of a pseudotype (VSV-SARS-St19) at high titre. Green fluorescent protein expression was demonstrated as early as 7 h after infection of Vero E6 cells with VSV-SARS-St19. VSV-SARS-St19 was neutralized by anti-SARS-CoV antibody and soluble ACE2, and its infection was blocked by treatment of Vero E6 cells with anti-ACE2 antibody. These results indicated that VSV-SARS-St19 infection is mediated by SARS-CoV-S protein in an ACE2-dependent manner. VSV-SARS-St19 will be useful for analysing the function of SARS-CoV-S protein and for developing rapid methods of detecting neutralizing antibodies specific for SARS-CoV infection.
-
-
-
Virus entry into a polarized epithelial cell line (MDCK): similarities and dissimilarities between influenza C virus and bovine coronavirus
More LessWe have analysed the uptake of influenza C virus and bovine coronavirus (BCV) by a polarized epithelial cell line, Madin-Darby canine kidney (MDCK) cells. Both viruses use N-acetyl-9-O-acetyl-neuraminic acid as a receptor determinant for attachment to cells. Virus binding assays with immobilized proteins indicated that a glycoprotein of 40 kDa is the major surface protein containing the receptor determinant for the two viruses. MDCK cells grown on filters for permeable support were found to have differential sensitivity to infection by these viruses. Both viruses were able to initiate infection via the apical domain of the plasma membrane, but only influenza C virus also accomplished infection via the basolateral plasma membrane. The resistance of MDCK cells to BCV infection from the basal filter chamber was overcome when the cell polarity was abolished by maintaining the cells in calcium-free medium. This finding indicates that the resistance to basolateral infection by BCV is a property of the cell line and not due to a technical problem related to the use of filters. Our results indicate that two viruses which use the same receptor for attachment to cells may differ in their ability to enter polarized cells. The possible involvement of an accessory molecule in the entry of BCV is discussed.
-
